Canada's health system is facing increasing pressures where:
- Many Canadians do not have a family doctor or nurse practitioner they can see regularly.
- Emergency rooms are often overcrowded, leading to long wait times.
- There is a pervasive shortage of healthcare workers, including doctors and nurses, which is exacerbated by burnout and high levels of stress among existing staff.
- Patients experience inequities in receiving care.
Health systems need to rapidly learn and apply evidence to combat these pressures. And while efforts are being made to modernize the health system through digital tools, there is still a need for better integration and access to health information.
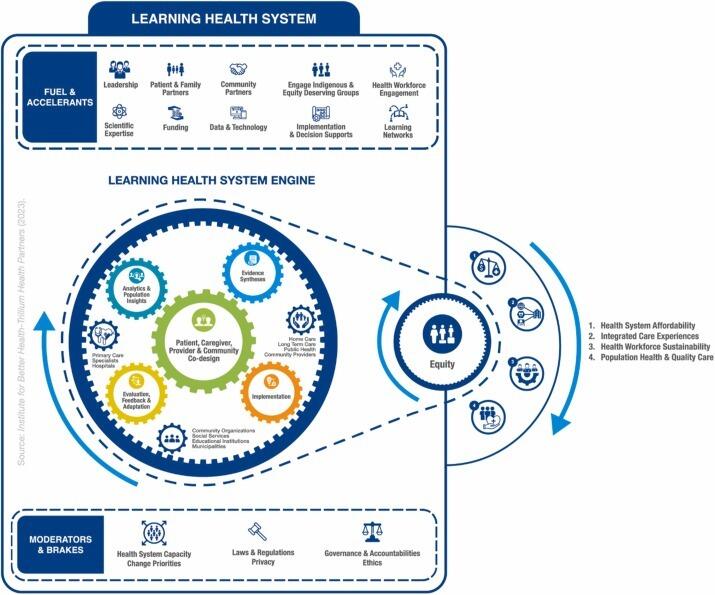
A Learning Health System (LHS) blurs the lines between research and health care delivery by incorporating research into everyday care. Traditional research is often separate from clinical care and slow to impact practice, while knowledge translation moves findings into care but lacks the continuous feedback and integration that define an LHS. By using data and digital tools, LHSs make health information easier to access and share – helping health care providers, patients, administrators, and policy makers make more informed and timely decisions.

Reid et al., Actioning the Learning Health System: An applied framework for integrating research into health systems, SSM - Health Systems, Volume 2, 2024, 100010, ISSN 2949-8562, https://doi.org/10.1016/j.ssmhs.2024.100010.
LHSs leverage big data and informatics to improve the integration and accessibility of digital health tools, making health information more readily available to providers, patients, administrators, and policy makers. LHSs can significantly address the challenges faced by the Canadian healthcare system by fostering continuous improvement and innovation, helping to create a more efficient, equitable, and responsive healthcare system.
LHSs employ ‘big data’ from electronic medical records and qualitative sources to develop a comprehensive picture of a patient’s health needs, diagnostics, behaviors, communications, interventions, care processes, costs, and clinical outcomes. By utilizing data analytics, including artificial intelligence and machine learning, LHSs generate actionable insights to address individual and population health needs.
LHSs incorporate the latest evidence and successful strategies to implementation, evaluation, feedback and adaptation to inform rapid-cycle improvements.
LHSs directly engage those impacted by the problem at hand, including patients, caregivers, care providers, community members, healthcare professionals, managers, and health system operators. Co-design activities must consider cross-sectoral approaches and build trusting relationships, paying attention to power differences among participants, especially those from equity-deserving groups. Early engagement, expectation management, and assessing learning needs are crucial, along with removing barriers to engagement.
LHSs employ implementation science methods to systematically design interventions and improve health service effectiveness. This involves understanding current behaviors, identifying strategies for desired behavior change, and specifying implementation details.
LHS approaches rely on realist evaluation methods to measure the effectiveness of multicomponent interventions for specific patient populations under different conditions. Evaluations help identify and eliminate inefficient care processes, creating new capacity.